Healthy Nurse, Healthy Nation™ Blog - Improving Health Care Access For Survivors Of Sexual Assault
One in two women and one in three men have experienced sexual violence involving physical contact during their lifetimes, according to the Centers for Disease Control and Prevention (CDC). (Editor's note: these stats were updated 12/7/22).
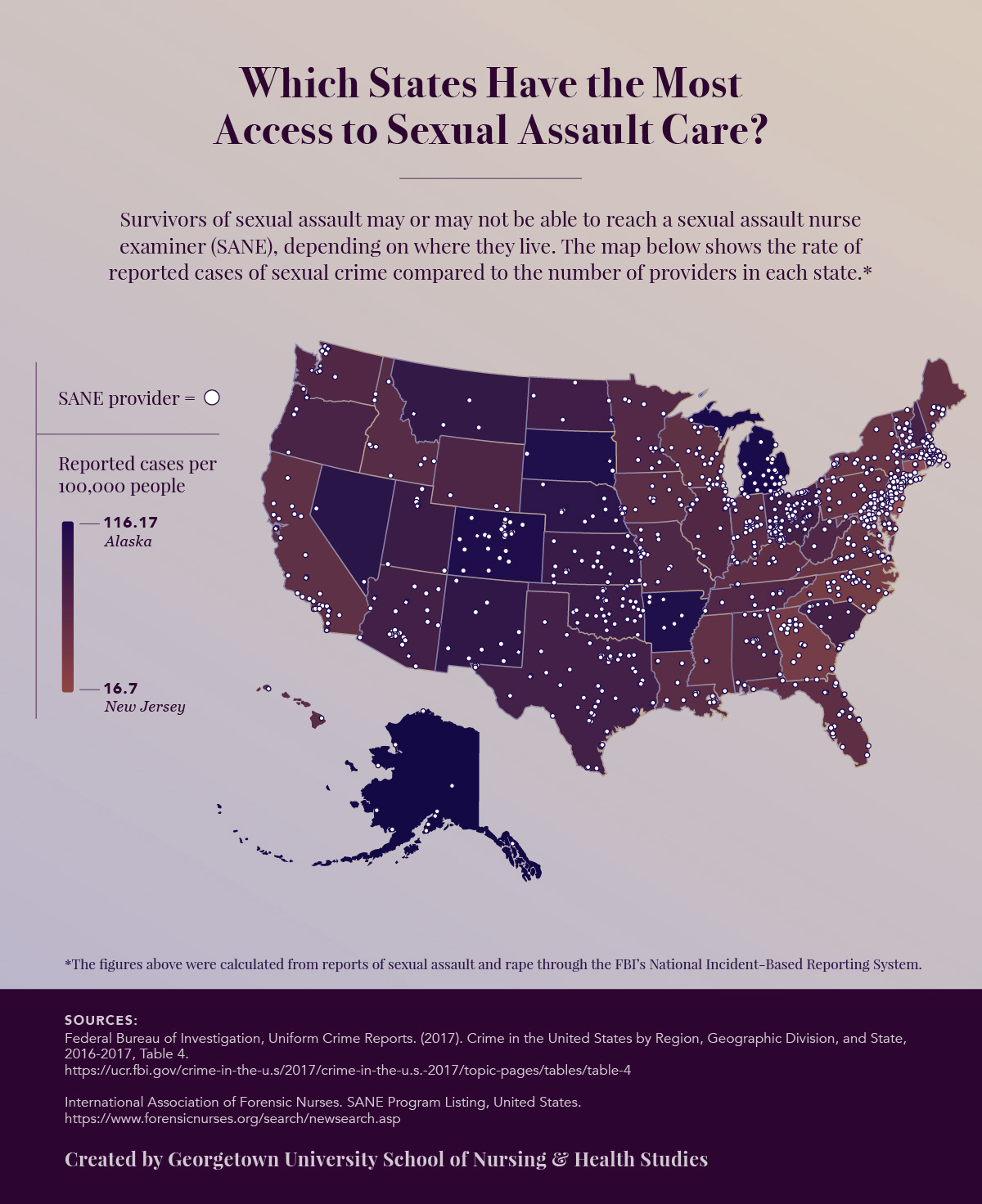
 This type of trauma necessitates urgent medical attention from trained sexual assault nurse examiners (SANEs), yet several obstacles exist for many survivors seeking specialized care. Depending on where a patient lives, he or she may have to travel for hours to reach the closest available provider for a Sexual Assault Forensic Exam (SAFE)—a critical step when a patient decides to report an assault to the police.
This type of trauma necessitates urgent medical attention from trained sexual assault nurse examiners (SANEs), yet several obstacles exist for many survivors seeking specialized care. Depending on where a patient lives, he or she may have to travel for hours to reach the closest available provider for a Sexual Assault Forensic Exam (SAFE)—a critical step when a patient decides to report an assault to the police.
“It’s very much a deterrent for rural [residents] to drive for any type of care,” said Pamela Biernacki, DNP, FNP-C, faculty member in the Georgetown University School of Nursing & Health Studies.
The gap in availability of appropriate care after a sexual assault affects the safety of individuals, families, and entire communities. Health care professionals, hospitals, and community stakeholders can make substantial improvements to SANE access.
Why do Survivors of Sexual Assault Need Specialized Care?There were 298,410 instances of sexual assault in the United States in 2016, as reported by the Bureau of Justice Statistics (BJS) in a bulletin on criminal victimization (PDF, 669 KB). External link When any survivor seeks medical attention after an assault, they require care that addresses both physical and mental health needs.
Triage often includes a forensic exam, which calls for specific equipment and a clinician trained to perform the assessment. To facilitate this specialized form of care, some hospitals have implemented SANE programs that staff certified nurses to treat patients who require interventions tailored to their needs.
Designated SANE facilities can make a difference in a survivor’s path to healing, from initial assessment and treatments to the criminal justice process (should the survivor choose to report the assault). Studies have shown that exams performed by SANEs “may result in better physical and mental health care for victims, better evidence collection, and higher prosecution rates,” according to a 2018 report on sexual assault and the availability of forensic examiners (PDF, 191 KB) External link from the U.S. Government Accountability Office (GAO).
The BJS bulletin indicates that many survivors choose not to involve law enforcement—nearly 80% of sexual assaults went unreported in 2016. However, receiving treatment from a SANE who fully understands a patient’s trauma can make a substantial difference regardless of whether the results of a forensic exam are used in a criminal case, said Michelle Metz, SANE Coordinator for Denver Health.
“Sometimes we’re the only person who is there,” said Metz. “We bear witness. We may be the only person who says ‘I’m really sorry this happened to you. I’m really glad you came in.’”
Survivors who are unable to seek care from a SANE-designated facility may miss out on the diagnosis and treatment of infections related to their assault, as well as emotional support and guidance on follow-up care, Biernacki said.
SANEs often provide survivors with referrals for mental health care. In her professional experience as a Nurse Practitioner, Biernacki has observed the long-term effects of trauma, particularly among women, who did not seek out treatment immediately following their assault.
“Depression and anxiety are the [most prominent conditions] I’ve seen,” she said. “It also comes out in physical symptoms, like insomnia or gastrointestinal problems.”
In some cases, women Biernacki spoke with did not fully understand their experiences, underlining the need for more education on what to do in the case of a sexual assault.
“Until we had a conversation after taking a thorough sexual history, [patients] didn’t realize that what they experienced is considered assault,” she said. “They had not identified it or did not want to take that emotional step to say, ‘Yes, I have been sexually violated.’”
How Many Sexual Assault Programs Are There?
Despite the prevalence of sexual assault in the United States and the need for SANE intervention, access to specialized care for survivors of sexual assault is limited.
The International Association of Forensic Nurses (IAFN) database of SANE providers External link shows that there are approximately 959 programs that offer SANE care in the United States. IAFN reported that 1,732 nurses are SANE-certified through their organization. External link Of those, about 1,230 nurses are SANE-A certified, meaning their training is specific to adults and adolescents, and 502 are SANE-P certified and are trained to work on pediatric cases. Approximately 381 nurses are dual-certified. (Editor's note: the information in this paragraph is outdated but the links will lead to the most updated information).
Nonetheless, research has shown that survivors lack access to SANE care. The GAO’s 2018 report on sexual assault and the availability of forensic examiners (PDF, 191 KB) External link reflects data from six states that served as case studies. Officials in every state reported a shortage of SANE providers, especially in remote areas.
“When you’re in some place like rural Colorado, the closest SANE program could be 100 miles away, or a two-hour drive,” Metz said.
Distance is a significant barrier for an individual who wants to be treated by a sexual assault nurse examiner. In a 2018 hearing on the availability of forensic exam kits in hospitals, External link New Jersey Congressman Frank Pallone Jr. explained that a survivor “must avoid bathing, showering, using the restroom, or changing clothes, or else risk damaging the evidence before it can be collected.”
These recommendations for preserving evidence leave an individual who lives hours away from a SANE-designated hospital with the options of experiencing extreme discomfort, risking the outcome of their forensic exam, or not receiving specialized care at all.
Go to a tabular version of data on states ranked for the most- and least-reported number of cases of sexual assault per facility. (Editor's note: this link is no longer active as of 12/7/22).
What is Causing the Shortage of Sexual Assault Nurse Examiners?
A number of factors contribute to the scarcity of SANE care. Based on its findings, the GAO report on sexual assault and the availability of forensic examiners (PDF, 191 KB) External link cited the following three barriers to increasing accessibility to SANE programs.
Lack of Funding from Hospitals or Law Enforcement
Officials in five of the six states selected for the GAO case study reported that obtaining support from key stakeholders was a challenge. For example, hospitals may be reluctant to cover the costs of training SANEs or to pay for SANEs to be on call.
Limited Availability of Training
In five of the six states, officials reported that the diminished availability of classroom, clinical, and continuing education training opportunities is a challenge to maintaining a supply of SANEs.
Clinical training requires 300 hours of SANE-related practice, which can be an obstacle in areas with smaller patient populations, said Jennifer Pierce-Weeks, CEO of IAFN.
“It can be difficult to establish competency as a sexual assault nurse examiner,” she said. “The classroom training [can be done] online or in-person, but then there is the clinical training which can be difficult for people to access.”
Low Retention Rates of SANEs
Officials in one of the selected states reported that while the state trained 540 SANEs during a two-year period, only 42 were still practicing in the state at the end of those two years, as a result of the challenges of working in a trauma setting.
Metz explained that in her experience as a SANE coordinator, “the nurses who do this work last either 18 months or more than five years.”
Biernacki emphasized the importance of establishing support systems for nurses, something that can be a challenge for smaller, rural facilities.
“With any type of burnout, it is about having that support,” she said. “But since [nurses] typically do work alone or have very few individuals that are part of that team, how do they build that sense of community and support?”
What Can Be Done to Improve Health Care Access for Survivors of Sexual Assault?
In the effort to improve access to sexual assault care, Biernacki said a good first step is to further educate student clinicians about this specialty and the needs of sexual assault survivors.
"We have started teaching about human trafficking, and we talk about intimate partner violence," she said. Delving further into sexual assault would be an appropriate next step.
While there are currently no national guidelines on sexual assault care, state and federal legislators are making efforts to make this type of health care more accessible.
In 2018, the Survivors' Access to Supportive Care Act (SASCA) External link was re-introduced in the U.S. Senate to expand access to qualified examiner services and develop national standards of care for survivors of sexual assault.
How Would SASCA Address Access to Specialized Care?
SASCA is endorsed by a number of health care and advocacy organizations, including IAFN. Pierce-Weeks explained how the main points of action presented in SASCA bill would help increase access to SANE care in the United States (PDF, 361 KB). External link
Evaluate state-level needs to strengthen the sexual assault examiner workforce.
SASCA will authorize $2 million per year for state-level surveys to better understand the following:
- Barriers to accessing sexual assault care and services.
- Availability of sexual assault examiners.
- Costs of training.
- Spectrum of state-training requirements and standards.
- Status of funding at the state level for sexual assault examinations.
“The idea is we would begin to have some data out there about what is truly available, what is not available, and where the highest needs are so that folks can begin to address those needs. It's movement in the right direction,” said Pierce-Weeks.
Develop and test national standards of care for survivors.
SASCA would direct the Department of Health and Human Services (HHS) to establish a pilot training and continuing education program for sexual assault examiners to be tested and incorporated by health care providers nationwide.
“If you work in a rural community, you’re maybe only taking care of five sexual assault patients a year,” said Pierce-Weeks. “Functioning in the role of the sexual assault nurse examiner, you’re really providing that comprehensive level of care, so competency can be an issue. What SASCA attempts to address is ongoing training and competency needs for sexual assault nurse examiners.”
Increase access for rural and tribal communities.
SASCA provides training grants to entities that serve rural and tribal communities, with 15% of the funding allocated for these grants set aside for Indian-affiliated organizations. SASCA also calls for the development of tools and best practices that will address the unique features and cultural sensitivities within rural and tribal communities.
“Alaska Native and American Indian populations across this country have much higher rates of sexual violence. They are a population in great need of services. This begins to address some of the challenges in those communities,” Pierce-Weeks said.
Increase understanding and access to sexual assault care nationwide.
SASCA will establish a pilot grant program to expand medical forensic exam training and services to new providers, as well as expand access in rural areas. SASCA will also establish a national sexual assault taskforce of government agencies and other stakeholders to better understand sexual assault and address the gaps in care for survivors.
“Like most nursing associations, we collect data, but we collect data based on the willingness of our members to submit that data. SASCA puts the onus on the state to identify where they have access problems,” Pierce-Weeks said.
Posted with permission from Nursing@Georgetown, the online Women’s Health Nurse Practitioner program from the Georgetown University School of Nursing & Health Studies.
Reviewed 12/7/22


Post a Comment or Question